Home
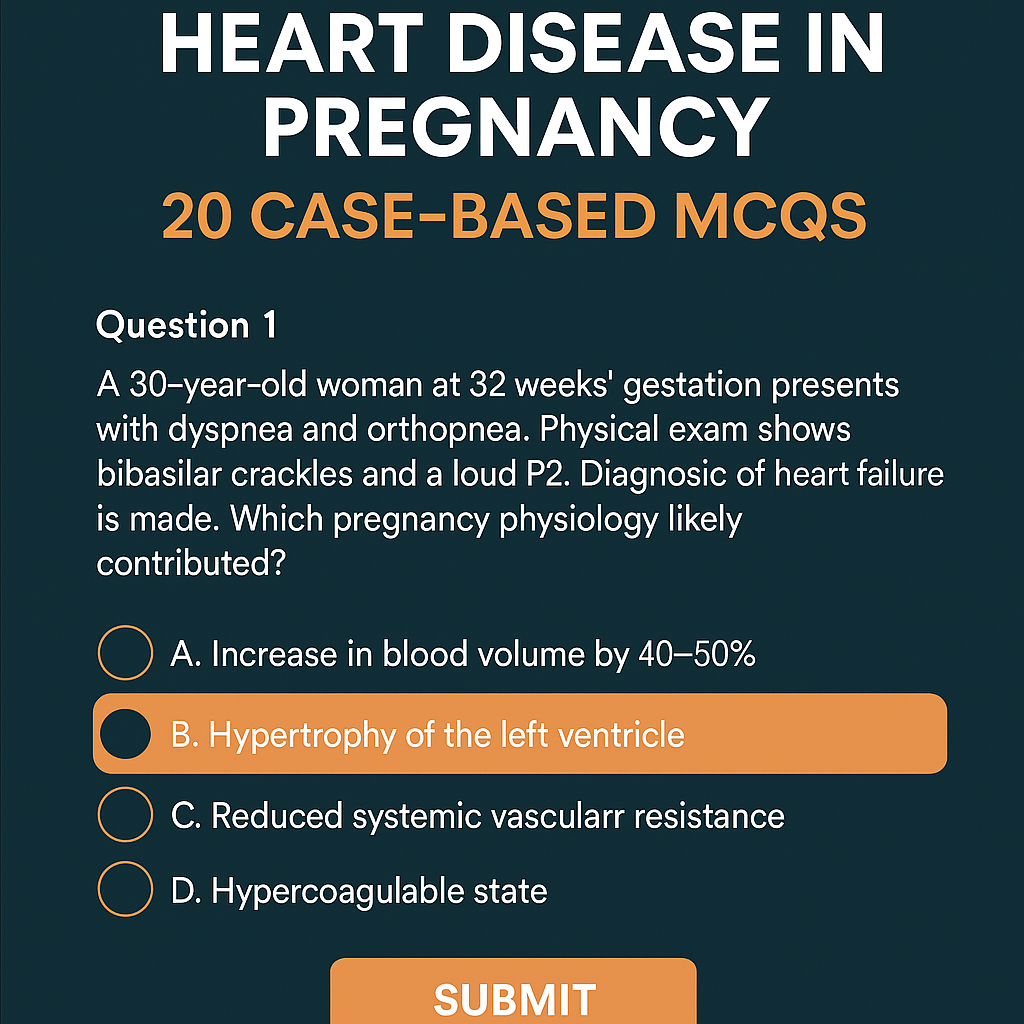
Heart Disease in Pregnancy: Causes, Risks, Management & 20 Case-Based MCQs (With Answers & Explanations) Below is a **complete, exam-ready, concise-but-exhaustive reference** for **Heart Disease in Pregnancy** — covering definition, physiology, classification, clinical features, investigations, management (stepwise), drug details, labor/delivery planning, postpartum care, and contraindications. HTML Versions