Home
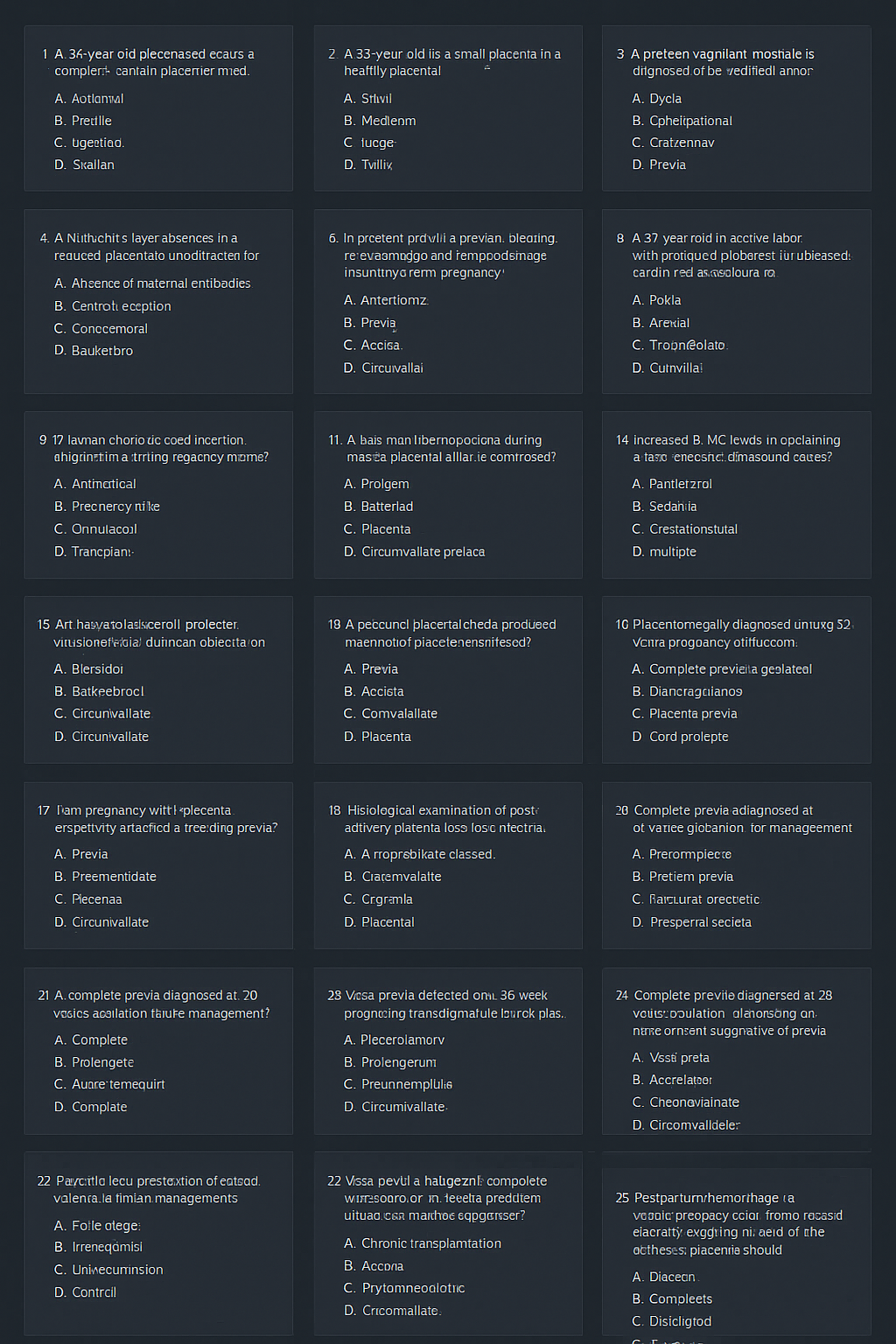
Human Placenta Case-Based MCQs | 25 Hard NEET PG & INI-CET Questions 2025 | Placental Anatomy Physiology Pathology --- HTML Versions